Medication-assisted treatment (MAT) is one of the most effective ways to treat addiction to drugs or alcohol. Since methadone was introduced in the 1970s, MAT has proven its effectiveness and become a sought-after way for people to regain sobriety and lead productive lives free of addiction. Alongside methadone, two new medications have been establishing their effectiveness at helping people overcome addiction to opioids — Subutex® and Suboxone®.
These medications are very similar, and you may be wondering how they differ in terms of side effects, usage and more. Both contain the drug buprenorphine as the main ingredient, and both are highly effective at helping people maintain sobriety. However, there are some differences worth noting that can help you identify which treatment is appropriate for you.
Read More About Buprenorphine FAQ’s Here
What Is Buprenorphine?
Buprenorphine is a semi-synthetic opioid. It is synthesized from a compound called thebaine, which occurs naturally in the opium poppy. Buprenorphine is an opioid partial agonist, so it binds to the same receptors in the brain as drugs like heroin and prescription painkillers like OxyContin®. However, the binding is only partial, so the maximum effects of buprenorphine are less than those of other drugs. This “ceiling effect” means that at a certain point, no further effect from the medication will be felt even if the dose is increased.
Low doses of buprenorphine produce enough of an agonist effect to keep the brain from launching an addicted individual into withdrawal when opioids of abuse are removed. With the painful symptoms of withdrawal avoided, a person on buprenorphine can function normally enough to participate in treatment. There are three stages of addiction treatment with buprenorphine:
- Induction: A physician begins administering buprenorphine when a person has stopped using opioids for 12 to 24 hours and is beginning withdrawal.
- Stabilization: After someone has discontinued or substantially reduced their consumption of the abused opioid, the physician will adjust the buprenorphine dose according to how the individual is responding.
- Maintenance: Once someone has found their optimal dose and is recovering well with buprenorphine, they will keep taking the medication for a length of time determined in consultation with their physician. Some people stay on buprenorphine for just a few months, and others remain on it indefinitely.
What Is Subutex?
Subutex is a brand-name medication containing buprenorphine. It comes in a sublingual tablet to be dissolved under the tongue. The Food and Drug Administration (FDA) approved Subutex alongside Suboxone in 2002, with the goal of providing an addiction treatment option with less abuse potential than methadone.
What Is Suboxone?
Suboxone is another brand-name medication that contains buprenorphine, but with one key addition — naloxone. Suboxone comes in a sublingual film as well as buccal forms that are meant to be held and dissolved between your cheek and gums.
What Is Naloxone?
The most substantial of the Subutex vs. Suboxone differences is that Suboxone combines buprenorphine with naloxone. Naloxone is an FDA-approved medication that can reverse an overdose by removing opioids from the receptors of the brain. Commonly known by the brand name Narcan®, naloxone comes in a nasal spray, as well as injections given into a muscle, under the skin or intravenously. Doctors can prescribe naloxone to patients participating in MAT or who are:
- Taking high doses of opioids for chronic pain
- Taking certain long-acting or extended-release opioids
- Receiving a rotation of opioid medications
- Being discharged from emergency care after an opioid overdose
- Completing mandatory detoxification or abstinence treatment programs
Naloxone is added to buprenorphine with the goal of reducing the potential for abuse. It is a full opioid antagonist, meaning it shuts down opioid receptors rather than exciting them.
If someone attempts to dissolve and inject a Suboxone film, the naloxone will trigger withdrawal symptoms immediately and block other opioids from attaching to the receptors for a period of time. However, if the naloxone wears off before the effects of other opioids taken, an individual could begin to experience symptoms of withdrawal again.
Subutex vs. Suboxone: Which Is Better?
When deciding between Subutex and Suboxone for addiction treatment, a common question is which one is better. Because they both contain buprenorphine, they perform the same function of preventing withdrawal and are equally effective at doing so. The only real difference appears if you attempt to abuse Suboxone.
If you are concerned about relapsing and abusing the medication or have experienced relapses in the past, Suboxone may be a better choice for you due to the abuse-deterrent features of naloxone.
Because Subutex contains only buprenorphine as its active ingredient, it is simpler to make and therefore less expensive than Suboxone, and is also available as a generic prescription.
Can Subutex Be Substituted for Suboxone?
Since Subutex and Suboxone share the same main ingredient, you may wonder whether you can substitute one for the other. As with any medication, you should never alter your dosage or try switching it out for another medication without consulting your physician. There is evidence that switching the medications leads to adverse effects.
In 2003, Subutex was Finland’s most abused opioid. To combat this issue, a high percentage of treatment facilities switched their patients from Subutex to Suboxone. A retrospective evaluation of the switch showed that switching the drugs at the same dose led to “adverse events” associated with withdrawal symptoms in half of the patients in the first four weeks. After four months, 26.6 percent of the patients reported adverse events.
Transferring from Subutex to Suboxone or vice versa should be carefully planned with your physician. You may suffer from certain withdrawal symptoms, and your dosage will likely need to be adjusted more than once to find the right level of the new medication.
Similarities Between Subutex and Suboxone
The buprenorphine present in both medications means they precipitate similar responses in the body. One of the most common questions asked is about the similarities between a Subutex high vs. Suboxone high. It should be noted that neither of these medications will produce a high if taken as directed.
Because buprenorphine treatment begins once withdrawal is in full swing, the person taking the medication may perceive the rapid reduction in painful symptoms as a high when it’s really just natural response associated with relief from withdrawal. Subutex and Suboxone both have the ceiling effect that prevents escalation of effects associated with a high after reaching a certain concentration.
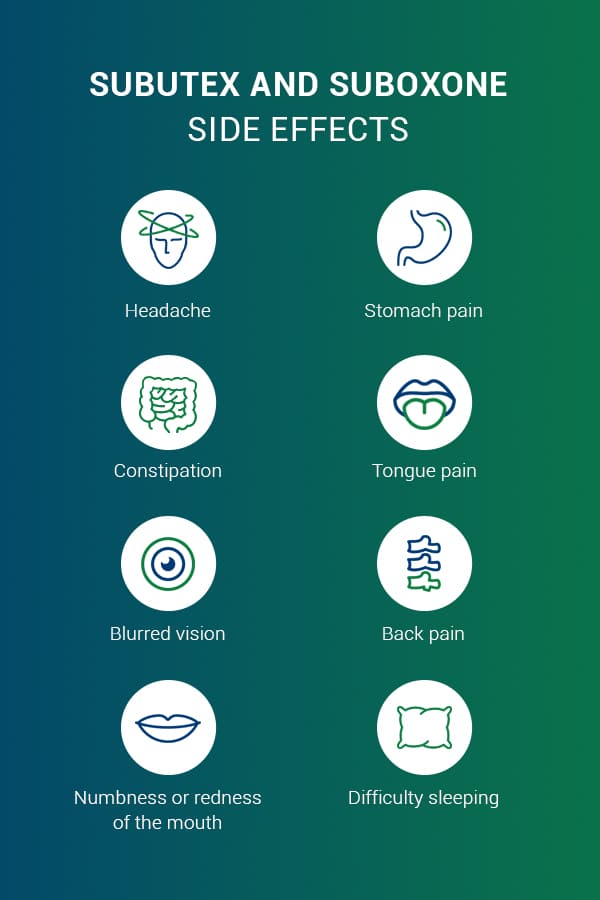
Subutex and Suboxone also have similar side effects, including:
- Headache
- Stomach pain
- Constipation
- Tongue pain
- Blurred vision
- Back pain
- Numbness or redness of the mouth
- Difficulty sleeping
These symptoms are usually mild to moderate. If they are severe or persistent, you should inform your doctor so you can determine together whether buprenorphine medications are appropriate for you.
The roles of Subutex and Suboxone in addiction treatment are the same. Taking either medication will assist your recovery in the following ways:
- Halt opioid withdrawal: Withdrawal is the obstacle that most frequently arrests a person’s recovery. By easing the symptoms, you decrease your chances of immediate relapse upon trying to quit.
- Eliminate opioid misuse: The ultimate goal of addiction treatment is to stop using an opioid of abuse. Subutex and Suboxone keep the brain from craving the drug, making it significantly easier to avoid relapse.
- Facilitate treatment: By suppressing withdrawal, these medications allow people to focus on their course of treatment rather than spending all their energy coping with the symptoms.
Subutex vs. Suboxone in Pregnancy
One serious concern is which medication is better for pregnant women to take. Buprenorphine now a more viable option for the treatment of women who are opioid-dependent during pregnancy. The American College of Obstetricians and Gynecologists makes it clear that buprenorphine-based medications have some benefits when compared to the historic go to for treatment medication for women during pregnancy, methadone. The benefits of buprenorphine over methadone for babies may include:
- Higher birth weight
- Larger head circumference
- Fewer preterm births
- Fewer neonatal withdrawal symptoms
Providers have historically recommended Subutex over Suboxone during pregnancy, due to the theoretical possibility of naloxone moving across the placenta to the baby. However recent studies have shown that very little placental transfer takes place, and multiple researchers have concluded that Suboxone is just as safe as Subutex for pregnant women when taken as directed.
Women with a history or high risk of relapse may elect not to take Suboxone due to its deterrent features. While the threat of being pushed into withdrawal by abusing Suboxone is enough to keep most people from attempting to inject it, this does happen on occasion. If a woman abuses Suboxone while pregnant, the withdrawal symptoms can cause serious problems in the pregnancy and lead to the baby suffering neonatal withdrawal upon birth.
Each mother-to-be should work closely with her medical providers to determine the treatment options and medications that are right for her and follow her treatment plan closely to ensure the best outcomes for her and her baby.
Tapering Off Of Subutex or Suboxone
Both medications, especially Suboxone, can be used in a maintenance program for as long as they are effective in recovery. Many people find that indefinite maintenance works for them, allowing them to live free of cravings for opioids of abuse like heroin. There is no maximum length of time you can be treated with buprenorphine.
Other individuals prefer to use buprenorphine as a stepping stone, with the ultimate goal of being completely medication-free. Either way, tapering off of any treatment medication, including Subutex or Suboxone is a process that must be carefully monitored by medical professionals. Even when taken as directed, buprenorphine may produce physical dependence. If someone abruptly stops taking one of these medications, they will start to experience:
- Shivering, shaking or trembling
- Muscle pain and cramps
- Nausea and vomiting
- Diarrhea
- Runny nose
- Watery eyes
- Hot and cold flashes
Additionally, they will experience strong cravings for opioids if a proper plan for tapering is not in place. If someone stops taking Suboxone because they have run out, for example, there is a danger that they will seek out their drug of abuse to stop the symptoms.
If you decide you want to stop taking Subutex or Suboxone, it’s crucial to inform your doctor and discuss a plan to do so safely. They will set up a tapering plan for you, in which you’ll take progressively lower amounts of the medication until you are off of it completely. This will minimize the symptoms you experience as your body readjusts to a complete lack of opioids.
When discussing potential treatment with a provider, think about whether you want to use buprenorphine as a maintenance medication or if you would rather start out with a plan to taper. Your doctor can help you make this decision based on the severity of your addiction.
Frequently Asked Questions About Subutex and Suboxone
Still have questions about buprenorphine-based medications for addiction treatment? You’re not alone. Here are five of the most common inquiries about Subutex and Suboxone.
1. Is Buprenorphine Treatment Just Substituting One Addiction for Another?
A: No. A successful MAT program using buprenorphine will reduce or eliminate the compulsive behavior, out-of-control drug use and constant drug cravings associated with addiction.
2. Who Can Prescribe Buprenorphine?
A: Any physician can prescribe buprenorphine for addiction treatment as long as they apply for and receive a special Drug Enforcement Administration (DEA) number. They must take an eight-hour class on treatment to apply, and can only treat 30 patients at a time for the first year after receiving their DEA number.
3. Are There Other Uses for Buprenorphine?
A: In its injectable form, buprenorphine can be used to treat pain. However, this is considered off-label use and is not currently common.
4. Can You Switch From Methadone to Buprenorphine?
A: Yes. Switching to buprenorphine may be desirable for people in recovery as methadone is generally taken every day on-site at a clinic, whereas Suboxone can often be taken at home by prescription. As with any mediation, consult your doctor and develop a plan for transitioning from methadone to buprenorphine.
5. What If I Miss a Buprenorphine Dose?
A: If you forget to take your Subutex or Suboxone, take it as soon as you remember. If it’s only a few hours until the time of your next dose, don’t double up or take more than your prescription.
Subutex and Suboxone Addiction Treatment With Health Care Resource Centers
Addiction to opioids is a serious condition that can wreak havoc on the body and even result in death by overdose. Seeking help for an opioid addiction takes immense courage, strong commitment and a treatment program that’s right for you. Health Care Resource Centers (HCRC) has more than 25 years of experience helping people overcome opioid use disorder through medication-assisted treatment.
In combination with counseling, case management and referrals to local resources, MAT provides individuals with a strong foundation for recovery and sustained sobriety. HCRC has a strong network of clinics located throughout New England, and a range of affiliate locations to serve clients in other areas of the country.
If you’re ready to take the next steps in your journey to freedom from opioid addiction, HCRC is here to help. Call us at (866) 758-7769, or send us your questions online. Stepping into recovery is a momentous decision. HCRC’s treatment and resources can help steady you on your new path to sobriety.